By Prof. Raphael Nyarkotey Obu
Women’s fertility declines after 35; science says 26 is the magic age for marriage.

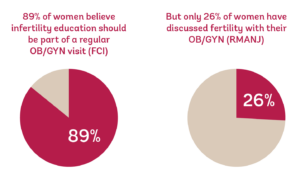
I read one article that states that the perfect age to get married, according to science is 26 for women and 32 for men. I decided to delve into this more due to the recent craze for fertility discussions on our airwaves. What could be the problem? I found that, though people are talking about fertility, they’re not having the conversation about where and when it matters. For instance, The RMANJ survey revealed that only 26% of women surveyed have had conversations with their OB/GYN about fertility and nearly half (42%) of women surveyed who had experienced infertility reported that their OB/GYN never started a conversation with them about fertility.
The magic number 26 for marriage
The number comes from the Algorithms to Live By: The Computer Science of Human Decisions, which was written by journalist Brian Christian and cognitive scientist Tom Griffiths. According to their book, people make the best decisions after screening 37 percent of the options.
They use the example of screening job applicants and argue that after looking through 37 percent of the people who applied, it would make sense to choose a candidate who was qualified without looking any further.
The authors of the study say that it’s at this point where the reviewers of the applicants have enough information to make a good choice, but not too much that they will get weighed down by indecision. The study further asserts that this rule works for picking out a partner. The range during which people typically look for love is between 18-40 and the 37 percent mark is 26. Past 26, the quality of the options begins to go down.
However, many experts seem to agree that the late 20s is the sweet spot for getting married. Psychologist Wyatt Fisher says that the reason this time in your life is so ideal for settling down is that it is at the point at which you have already completed your education and started a career.
Clinical social worker Kelsey Torgerson says it’s crucial to at least wait until the human brain is fully developed to find a life mate, which isn’t until age 25.
She says, “I believe it’s best to wait until this marker. It’s also important to experience stressors with your partner that you overcome, so if you have a high school sweetheart, you should see how you two handle college, long distance, studying abroad, or getting two jobs. You want to know that you have the conflict management strategies in place for a healthy, successful marriage down the road.”
Relationship therapist, Weena Cullins, thinks the magic number is 28. As she explains, “In my clinical experience, I’ve found that the best age to get married for women in the U.S. is 28. At age 28, my soon-to-be brides exhibit self-awareness and confidence in their choice of a mate. Most 28-year-olds have had the time to successfully explore who they are on a personal and professional level, discover the qualities they desire most in a life partner, and learn from mistakes they made in previous relationships. You’ve had time to get settled in a career, experience the college, and graduate school if that’s your preferred path, or simply live independently before combining your life.”
The Magic Number 32 for Men
And for men, Cullins thinks the magic number is 32: “Waiting until age 32 affords men an opportunity to get settled into a career and potentially pursue professional advancement before tying the knot. It also allows them to develop socially and emotionally through living on their own and dating. By 32, many men have spent enough time on the social scene to be able to make an informed decision about entering into married life. They also tend to have a sober perspective about having children and their role in co-parenting. This benefits the overall health of the relationship.”
Why the number 26 is important for women
A recent study by Owen and Sparzak, (2022) found that females are born with a determinate number of oocytes. In contrast to their male counterparts, females do not create new gametes throughout their lifetime. This number of oocytes peaks at around 20 weeks gestation and decreases with age. The female gametes decline stepwise until approximately age 32, at which point the number of oocytes decreases more quickly until about age 37 when they decrease significantly.
As modern women push the initial childbearing age back, age-related fertility decline is increasing among our population. Given this reality and that there is no cure for this phenomenon, the OBGYN Generalist has an important role in educating patients regarding their potential fecundity starting at an early age and referring patients for further workup promptly.
Age and eggs
- A woman’s age is the most important factor affecting her fertility and her chance of having a baby.
- The chance of having a child is much higher for women younger than 35 years and men younger than 40 years than for older women and men.
A woman is born with all the eggs she will ever have. As she ages her eggs age with her and their number and quality reduce over time. This is why her chance of having a baby also reduces over time, especially for women older than 35 years of age.
In one study, Andersen et al.(2000) looked at over 1 million pregnancies, women over 35 had a much higher rate of pregnancy loss; the risk of miscarriage for women over 40 was more than 50%, and by age 45, over 90% of pregnancies ended in miscarriage. Rates of Down syndrome increase significantly as well, from 1 in 1,200 for mothers aged 25 to 1 in 30 for mothers aged 45. So while 35 is not the single “age of fertility decline,” it makes sense as a convenient shorthand.
Age-related fertility decline is a universal and consistent biological trait for all women (and for men too, though the timeline is longer). Unfortunately, the age of fertility decline cannot be extended with a supplement, diet, exercise, or other therapies (though fertility decline can be steepened by certain lifestyle factors, such as smoking, or exposure to chemotherapy or other medications). In other words, women can’t extend their fertility through lifestyle changes or good habits that are beneficial to other areas of health (such as heart health, for example). That’s why egg freezing is such a powerful tool for women who want to preserve the option to have children later in life.
In another survey performed by Reproductive Medicine Associates(2016)of New Jersey in March, the gap between what people believe about their fertility and the actual biology is pretty wide.
The survey, which polled the beliefs of 1,000 adults between the ages of 18–40, demonstrated that 57% of respondents reported that they believed a woman’s “biological clock” stopped ticking at age 44. While it’s true that some women can have children naturally at age 44, fertility declines throughout a woman’s 20s and falls significantly after 35; only about half of women over 35 can achieve pregnancy in one year, compared with three-quarters of women under 31. By age 44, pregnancy rates are a mere 1–5%, with only about 2% of the remaining eggs deemed chromosomally normal. (Of course, the “biological clock” is an imperfect metaphor, but the fact remains that women have a very small chance of getting pregnant naturally over age 40.)
This survey is just the most recent in a series of studies examining public knowledge of fertility. Another recent survey performed by the Royal College of Obstetricians and Gynecologists in the UK examined the fertility perceptions of 1,000 young men and women between ages 16 and 24.
In this survey, more than 80% of both sexes believe women’s fertility only begins to decline after age 35. (As we talk about often, fertility decreases throughout our adult lives—it’s just the more drastic decline that sets in at 35.) Additionally, a quarter of young men thought a woman’s fertility only starts to decline after the age of 40 (compared with 16% of girls). And yet another 2016 survey, this one by the Fertility Centers of Illinois, revealed that of 1,208 American women ages 25–45 who had never been pregnant, only 48%—that’s less than half—understood that there was an age-related decline in fertility and increase in aneuploidy and pregnancy loss.
These recent results mirror those of the comprehensive 2011 study by pharmaceutical company EMD Serono that examined the fertility “IQ” of 1,010 women aged 25–35 who had never given birth and were not actively trying to conceive. Despite indicating that they plan to have their first child in their early to mid-30s, 73% of women in the Serono survey “anticipate that they would have an average, or easier than average, time conceiving than most women.” This belief doesn’t match reality: the survey reports remind us that 1 in 4 married women aged 35–44 experience infertility when attempting to have their first child, compared to only 1 in 10 of those under the age of 30.
Additionally, only a third of Serono’s respondents correctly identified age as the leading risk factor for infertility, and most believed that women over 40 have between a 10 and 40% chance of pregnancy in any given month—the actual monthly chance of pregnancy is only about 10%! The respondents also generally overestimated the success of IVF (believing IVF pregnancy rates to be 50–59% when they are 20–29%) and, importantly, were unaware of the importance of the age of the egg too in vitro fertilization success; 54% think that the chance of successful pregnancy via IVF does “not depend on the origin of the egg.”
How can this be?! It seems like everywhere we look, people are talking about fertility—but it turns out they’re not having the conversation where and when it matters. The RMANJ survey revealed that only 26% of women surveyed have had conversations with their OB/GYN about fertility and nearly half (42%) of women surveyed who had experienced infertility reported that their OB/GYN never started a conversation with them about fertility.
This again reflected the earlier EMD Serono survey results, which revealed that a majority of women never discussed future pregnancy plans (52%), age as an infertility risk factor (78%), or infertility treatment options (89–96%) with their OB/GYN. And it’s not because women don’t want this info; the Fertility Centers of Illinois reported that 89% of respondents agreed that infertility education should be mentioned at an OB/GYN visit and 52% of women age 35 or older stated that they would have made different life choices if they had known about the age-related decline in fertility.
Why aren’t women having this conversation with their doctors—before their fertility becomes a time-sensitive issue? Probably, it’s a combination of the fact that doctors aren’t always comfortable breaching the topic with patients (or there may not be a time in an otherwise packed OB/GYN visit); the fact that there’s still a stigma surrounding fertility issues, childlessness, and fertility preservation; and the fact that women can’t ask their doctors about a problem if they’re not aware of it in the first place.
That’s why some experts are calling for fertility education at the high school level, and why Adam Balen, Chair of the British Fertility Society, is advocating for “choice, not chance,” saying, “We aim to ensure that sex and relationship education not only covers how to avoid pregnancies and sexually transmitted diseases but also includes information about fertility and planning for the right time to start a family… We want to enable young people to make informed choices about pregnancy, whether that choice is to start a family or not.”
Credit: Extendfertility.com, 2016)
Men infertility
Age and sperm
Men younger than 40 have a better chance of fathering a child than those older than 40. The quality of the sperm men produces seems to decline as they get older.
Most men make millions of new sperm every day, but men older than 40 have fewer healthy sperm than younger men. The amount of semen (the fluid that contains sperm) and sperm motility (the ability to move towards an egg) decrease continually between the ages of 20 and 80.
We’ve all heard about men in their 80s and 90s fathering children, but this is rare. A father’s age also affects the chance of a couple getting pregnant. It takes longer for partners of men older than 40 years to conceive.
Assuming a woman is younger than 25; if her partner is also younger than 25, it takes an average of five months to get pregnant. If her partner is older than 40 years, it takes around two years, and even longer if he is older than 45.
Also, the risk of miscarriage is higher for women whose male partner is older than 45, compared to men younger than 25 years of age. For couples having IVF, the chance of having a baby is higher if the man is younger than 41 years of age.
Take Home
A concern for many women entering their 30s and beyond is when their fertility potential will begin to decline.
Studies show conclusively that older women suffer more fertility problems than younger women. In our society especially, where women pursue rewarding careers and often delay childbearing in the process, deciding when to pursue pregnancy while facing a ticking “biological clock” can be a daunting choice.
The American College of Obstetricians and Gynecologists (ACOG) recently updated its committee opinion, stating that women’s fertility begins to decrease gradually but significantly beginning at approximately age 32 and decreases more rapidly after age 37. Women older than 35 should receive an expedited fertility evaluation and undergo treatment after six months of failed attempts to conceive. In women older than 40 years, more immediate evaluation and treatment are warranted.
While there is no single age that represents a “fertility deadline,” conclusive data shows that the chances of achieving pregnancy are linked with age and decrease with increased age. However, the rate of this decline is relatively modest up until the early 30s. The reasons for this are many, but they center on the concept that increasing maternal age is generally associated with a decline in both the number of eggs and the quality of those eggs.
Women need to understand the effect of age on fertility, especially when they would like to plan a family. In most cases, an evaluation performed by an infertility expert can shed light on the “ovarian reserve,” a term used to describe how many eggs are available every month. In many instances, other problems are also diagnosed during such an evaluation to increase non-age-related issues that may be causing problems.
NB:
Prof. Nyarkotey has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations to justify his write-ups. My articles are for educational purposes and do not serve as Medical advice for Treatment. I aim to educate the public about evidence-based scientific Naturopathic Therapies.
The writer is a Professor of Naturopathic Healthcare, a Medical Journalist, and a science writer. President, Nyarkotey College of Holistic Medicine & Technology (NUCHMT), African Naturopathic Foundation, Ashaiman, Ghana. E. mail: [email protected].